|
| https://www.recorder.com/Arts---Culture-Calendar-Oct-11-to-Oct-17-2018-20734283 |
One question I get asked a lot through email and on my Facebook page is whether surgery for PF is worth it. That depends on a few things:
- Everyone is different. PF surgery may work for one person and not the next.
- What else have you tried? Have you tried cortisone injections? Physical therapy? Custom orthotic inserts? Oftentimes surgery isn't necessary because these methods can provide relief from PF.
- What kind of surgery you have. I had the Tenex procedure. Some surgeries are more successful than others. That is something you will want to discuss with your doctor.
- How long you wait before having surgery. Most doctors will want to wait until all other options are exhausted before trying surgery, if they even agree to it at all. But, as my doctors have told me, the longer you wait to treat PF, the harder it is to get rid of it.
If you are considering surgery to treat your PF pain, I will repeat what I said in my last post: yes, I do think surgery is helpful.
The last time I wrote a post, in July, I had only just started feeling better. I was still doubtful of my success with surgery overall. In a little over two weeks, it will be one year since my surgery. I figured this would be the perfect time to let you all know that I am so glad I went through with it!
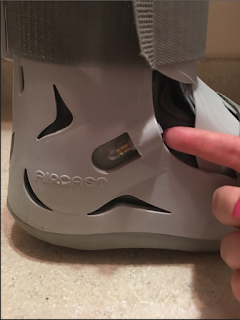
At this time last year, I was in an incredible amount of pain. I'd been wearing a walking boot (or Franken-boot, as I called it) for a few months. I could hardly walk, let alone stand for very long. Even driving wasn't easy. I no longer have those problems.
Here are the best things about having had surgery, almost a year later:
- It feels like I don't have PF at all most days. That's not to say that the pain is 100% gone; it isn't. If I have a long day of walking (and by long I mean a few miles or more) or standing, I will still be in a great deal of pain. But I don't feel it with every single step that I take, as I used to.
- I can wear shoes other than sneakers! (But I got so used to wearing sneakers that I still wear them most days. 😆) I have worn flip-flops, flats, short heels, boots, etc., all with very minimal pain. I no longer wear my orthotic inserts or heel lifts. My doctor probably wants me to still wear them (and I should, considering PF could come back), but I haven't in months. If you do have surgery, you will want to ask your doctor how long you should continue wearing your insets afterward.
- As my right foot (the foot which was operated on) got better, so did the pain in my left. At one time the pain in both feet was equally severe. My doctors and physical therapist suggested this was probably because I limped for so long (leaning on my left side to relieve the pain in my right foot.) In doing so, I developed PF in my left foot. Most days, like my right foot, there is little to no pain at all in my left foot.
- I no longer have to turn down fun plans with family and friends because of the pain in my feet. This by far is the greatest success I have had with surgery. There were so many things I missed out on before my surgery - pretty much anything that involved lots of walking and long periods of standing. I'm so thankful I don't have that problem anymore.
If you have had surgery for PF, was has been your experience? What procedure did you have? Did you have success? Any reduction in pain? Please let me know!
In my next post, I will talk about heel lifts and how they can help relieve PF pain.
I can be reached with any questions on my Facebook page: https://www.facebook.com/plantarwhat/
or through email: wsmalls12194@gmail.com.
Thanks for reading,
Becky
In my next post, I will talk about heel lifts and how they can help relieve PF pain.
I can be reached with any questions on my Facebook page: https://www.facebook.com/plantarwhat/
or through email: wsmalls12194@gmail.com.
Thanks for reading,
Becky