https://www.shutterstock.com/video/clip-4544480-stock-footage-waking-up-from-surgery.html
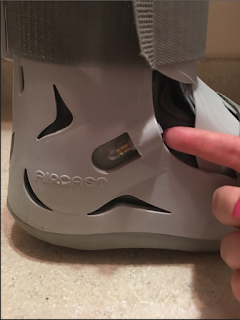
Before I was released from the hospital, I was shortly kept for observation to make sure I came out of anesthesia okay and didn't have any other complications. Dr. Shah had wrapped my foot in Ace bandages told me to wear my walking boot until I got home. As I was getting dressed and ready to leave, I didn't feel any pain at all, hardly. In fact, I was able to put pressure on my foot right away, getting in and out of the car and into my apartment.
I was more tired than anything when I returned home, having been awake since 6 AM that morning, and went right to bed to nap. Per Dr. Shah's instructions, I kept my foot elevated with pillows and blankets. I was given Oxycodone for pain, of which I was to take 1 to 2 tablets every 4 to 6 hours as needed. I only needed the painkillers the first 3-4 days or so. They worked (wonderfully) at eliminating the pain those first couple days, but were not without side effects. I became very bloated and constipated, even after drinking plenty of water and Metamucil and eating fibrous foods. They also made me drowsy and a little dizzy (I am prone to vertigo, so that wasn't unexpected.) I was not able to take ibuprofen (such as Advil) or Naproxen (like Aleve, which Dr. Shah had prescribed me for PF pain.) When I stopped taking Oxycodone, I was able to take acetaminophen (Tylenol) for pain. Once I tapered off the Oxycodone, the side effects I'd had subsided.
The hardest part of my recovery was walking. Every recovery is different, but for me, walking or putting even the slightest amount of pressure on my foot was incredibly painful. My doctors insisted that it was okay for me to walk, and even encouraged me to do so, but it was, at times, nearly impossible. The first few days, I hobbled to and from the bathroom with intense pain, holding onto doors and furniture (and my boyfriend) to maintain my balance. Finally, I'd had enough and decided to get crutches, which were a lifesaver. If your pain is as intense as mine was after surgery, I highly recommend getting them. It's important to the healing process to put a little pressure on your foot, but if you're struggling just to walk to the bathroom and fridge, don't suffer. Get crutches.
https://www.amazon.com/DMI-Crutches-Adjustable-Handgrips-Accessories/dp/B000CSQJBY?th=1
The other part of recovery that was particularly hard was showering. I was told not to get my foot wet. As you can imagine, it was nearly impossible to stand on my good foot in the shower without losing my balance and soaking my bandages, so a shower stool was a must for me. I sat on the stool with my wrapped foot sticking out of the shower. I've heard of some people wrapping their feet with plastic bags or garbage bags to ensure that no water gets under the bandage, but I didn't find this necessary. Here is a link to a shower stool like the one I used: https://www.amazon.com/Tool-Free-Assembly-Adjustable-Anti-Slip-Stability/dp/B06ZYW53V5/ref=sr_1_1_sspa?ie=UTF8&qid=1526314164&sr=8-1-spons&keywords=shower+stool&psc=1
If you get surgery for your PF pain, you won't be able to drive for a while. I wasn't able to drive for at least two weeks, because it was my right foot that was operated on. Be ready to spend a lot of time in bed or on the couch with your foot elevated. There's not much to do, so I recommend using the down time to read a book (or a couple, if you're an avid reader like myself), get into a new Netflix show or documentary, or do Sudoku and word searches like I did. I wasn't as ready for all the free time as I thought, and went stir crazy pretty quickly! The first time I went out was to a store (with my crutches and walking boot, driven by a friend) toward the end of the second week. It was probably the most exciting shopping trip I'd had in a long time, after being cooped up for so long!
https://collegecandy.com/2015/02/23/going-out-in-winter-pros-and-cons/
Looking back on those first few days after surgery, I can say the recovery wasn't as bad as I'd expected. Having help and support from family and friends is very important, as well as listening to your body. No one knows your body better than you do; if you feel something isn't right, or you feel like you're in too much pain, talk to your doctor. Keep them updated on how you're doing. If you're struggling to walk, ask your doctor about using crutches until you can move comfortably on your own. Do whatever you need to get better.
In my next post, I will discuss the weeks and months following surgery, including follow-up appointments with my doctor, and how I am doing now, 6 months later. As always, I can be reached on my Facebook page, https://www.facebook.com/plantarwhat/ or via email (wsmalls12194@gmail.com) to answer any questions.
Thanks for reading,
Becky